Scientists raise alarm as drug-resistant fungus with 50% death rate spreads across six continents

The world's most feared hospital microbe has proteins in its cell walls that let it stick 'like glue'
Don't Miss
Most Read
Latest
Scientists are sounding the alarm over a deadly fungus that's spreading across the globe at a worrying pace.
Candida auris, a drug-resistant yeast first spotted in a Japanese patient's ear canal back in 2009, has now reached at least 61 countries spanning six continents.
The infection can cause significant harm to anyone with a weakened immune system. Even when patients receive antifungal treatment, more than half don't survive.
The fungus became a serious public health concern after reaching India in 2014, and a new scientific review warns it's only gaining strength as it continues its global march.
TRENDING
Stories
Videos
Your Say
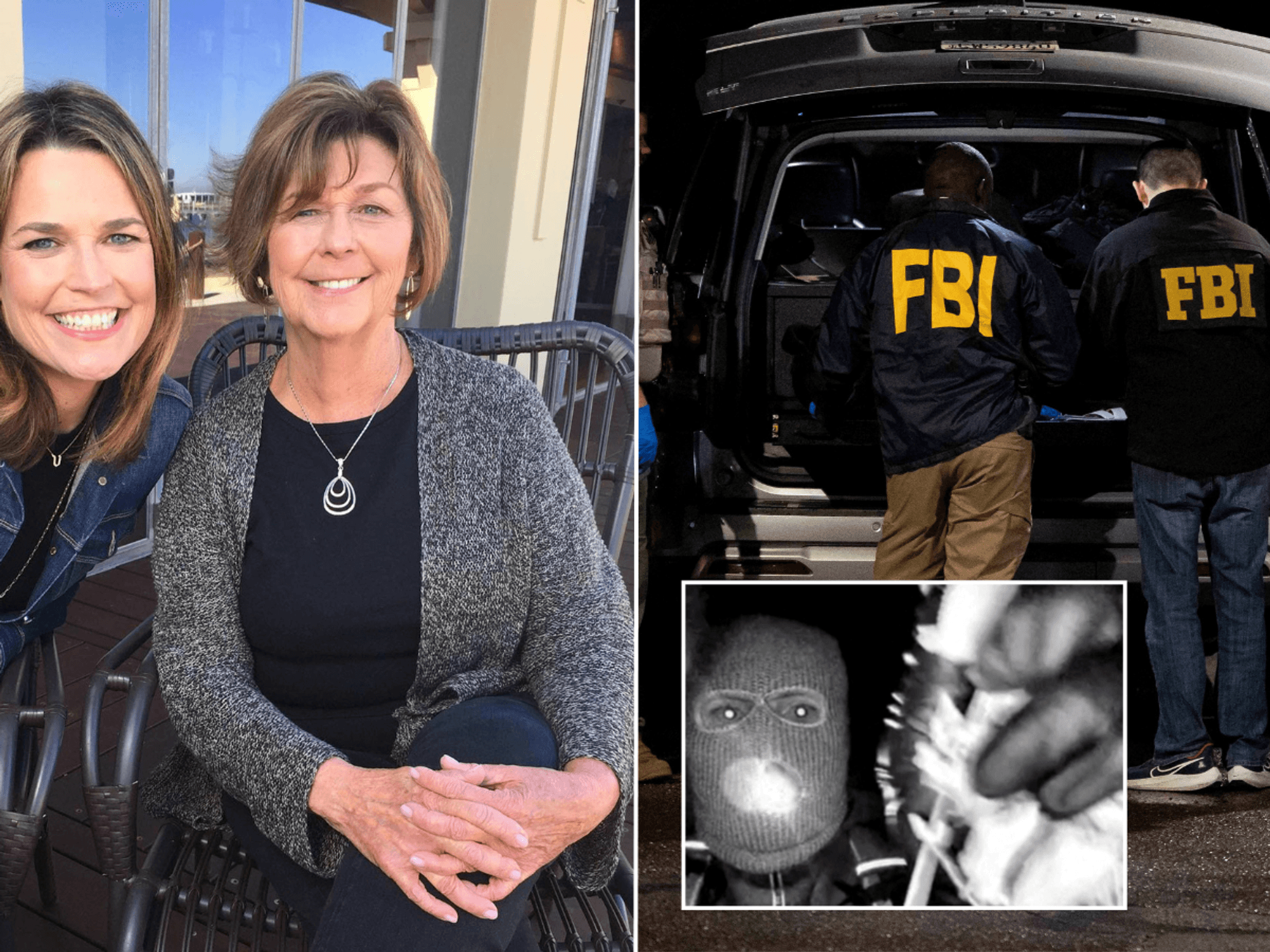
The fungus has special proteins in its cell walls that let it stick 'like glue'
|GETTY
What makes this fungus so dangerous?
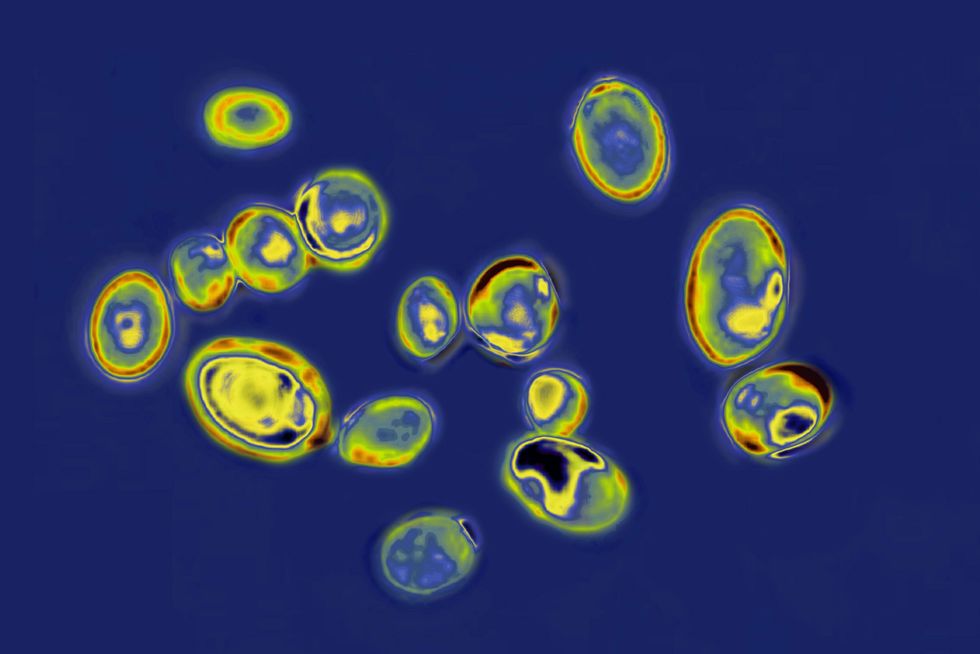
According to scientists, the yeast can transform itself, switching from its typical form to one that spreads through filaments, which helps it develop drug resistance at an alarming rate.
Another concerning behaviour of the fungus is how it latches onto the skin. The fungus has special proteins in its cell walls that let it stick "like glue" and set up camp on patients.
This creates a problem in hospitals, because once a person becomes colonised, they can unknowingly pass the infection to other patients, both within their own hospital and when transferred elsewhere.
The fungus has another defence mechanism that makes treatment incredibly difficult. It's equipped with tiny pumps on its cell membrane that essentially flush out antifungal medications before they can do their job.
LATEST DEVELOPMENTS
On top of that, Candida auris clumps together to create slimy biofilm layers on surfaces, which stops drugs from getting through properly.
In addition, doctors face the hurdle of mistaking the fungus for other conditions, which means patients don't get the right antifungal treatment quickly enough.
Scientists still aren't entirely sure whether there are additional ways the fungus manages to dodge our current medicines.
Meanwhile, Trichophyton indotineae has emerged as a growing concern on British soil, despite being virtually unheard of in the country three years ago.
Figures presented at the ESCAIDE conference in Poland last week revealed a dramatic escalation. Recorded cases jumped from just 44 prior to 2022 to 258 by March this year.
"It's becoming a really big problem in the UK," Professor Darius Armstrong-James from Imperial College London told The Sun.
The fungal specialist voiced significant worry about the frequency of new hospital cases, though he acknowledged uncertainty regarding whether the infection could become endemic or reach pandemic proportions.
The UK Health Security Agency has confirmed it is monitoring the increase in antifungal-resistant Trichophyton indotineae infections.
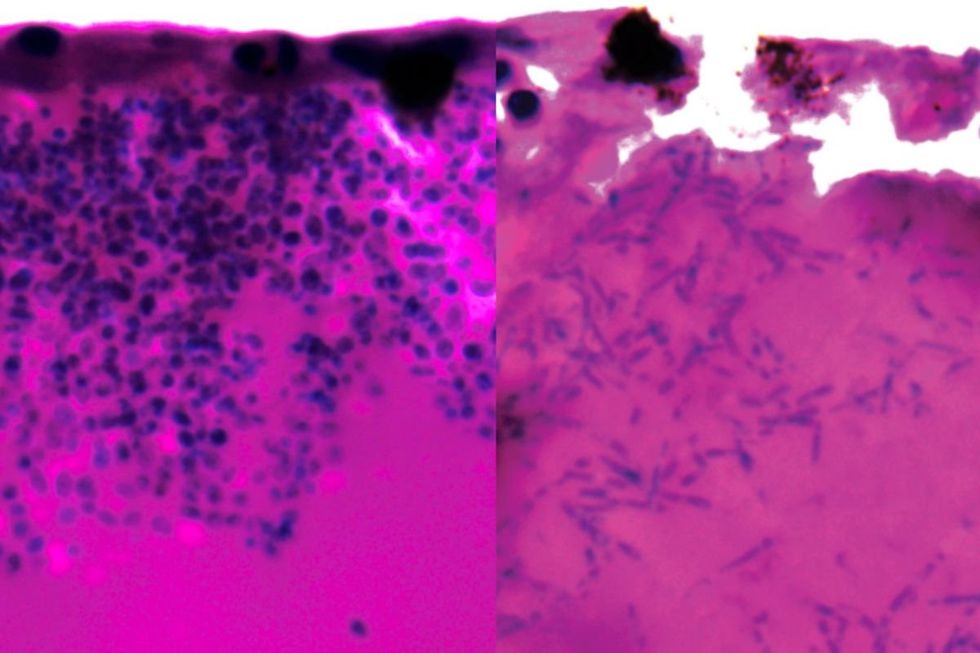
Candida auris during infection, with the right image showing filaments
|GETTY / UNIVERSITY OF EXETER
The pathogen originally appeared in India in 2014 and has since spread to more than 20 nations globally.
Treatment presents considerable challenges for patients, as those infected must undergo extended hospital stays while receiving itraconazole, the primary medication used to combat the condition.
However, this treatment carries substantial dangers, producing severe toxic effects affecting both cardiac function and liver health, adding another layer of complexity to managing increasingly resistant fungal infections.
Our Standards: The GB News Editorial Charter