Covid could trigger new allergies years after infection, scientists warn with risk rising by up to 74%

'Long Covid is, at its core, a condition of immune dysfunction'
Don't Miss
Most Read
Growing evidence suggests coronavirus infection may trigger the development of new allergies, adding another burden for the estimated 20 million Americans currently living with long Covid.
Research indicates individuals who contracted the virus face a substantially elevated risk of developing allergic conditions. Studies show the likelihood of new allergies increases by between 20 and 74 per cent, depending on the specific condition.
Asthma, allergic rhinitis, and food sensitivities are among the most commonly reported new-onset conditions in patients recovering from coronavirus infection.
Scientists have identified immune system dysfunction and mast cell activation syndrome as primary mechanisms driving these allergic responses.
TRENDING
Stories
Videos
Your Say

Allergic rhinitis is among the most common conditions affecting patients recovering from Covid
|GETTY
Vaccination appears to offer some protection against developing these post-infection allergic conditions, according to researchers examining electronic health records from millions of patients.
Research published in Nature Immunology last December examined blood samples from individuals who recovered fully from acute infection compared with those experiencing prolonged symptoms.
The findings revealed that long Covid is linked to persistent immune dysfunction, marked by ongoing inflammation, exhausted immune responses, and disrupted cellular energy processes.
"While we have not examined allergies in our long Covid cohorts, it is plausible that SARS-CoV-2 infection could contribute to increased allergic responses," said Malika Boudries, PhD, an assistant professor of medicine at Harvard School of Medicine and the study's lead author.
She noted this theory is bolstered by emerging data connecting coronavirus to immune disruption, autoimmune phenomena, and reactivation of dormant viruses like Epstein-Barr.
Ziyad Al-Aly, MD, chief of research and development at the VA St Louis Health Care System, described mast cell activation syndrome as integral to long Covid rather than a separate condition.
A separate study in the Journal of Allergy and Clinical Immunology analysed electronic health records from over 118 million patients in the United States.
Researchers tracked new diagnoses of respiratory and inflammatory conditions during a three-month follow-up period after coronavirus infection.
LATEST DEVELOPMENTS
The results showed patients who had contracted Covid were 74 per cent more likely to develop chronic rhinosinusitis, 66 per cent more likely to receive an asthma diagnosis, and 37 per cent more likely to develop allergic rhinitis.
"Covid infection is associated with a heightened risk of respiratory type 2 inflammatory diseases, whereas vaccination appears protective," the researchers reported.
Those who received vaccinations but avoided infection showed considerably reduced risks for asthma and chronic rhinosinusitis, with modestly lower rates of allergic rhinitis as well.
Clinicians at specialist centres across America report seeing these allergic manifestations firsthand in their patients.
"Long Covid is, at its core, a condition of immune dysfunction," said Jacqueline H. Becker, PhD, an assistant professor at the Icahn School of Medicine at Mount Sinai. "New allergies are one manifestation of that dysfunction."
Lisa Sanders, MD, medical director for the Yale Long Covid programme, has observed childhood asthma returning with force in patients following infection.
"I have seen many new cases of asthma, or patients who had asthma as a child, which had been quiet for many years and came roaring back after their Covid infection," she said.
David Putrino, PhD, director of rehabilitation innovation at Mount Sinai, has documented sensitivities to gluten, high-histamine foods, perfumes, and cleaning products among his patients.
Monica Verduzco-Gutierrez, MD, who chairs the Department of Rehabilitation Medicine at UT Health San Antonio's long Covid clinic, attributes these conditions to immune dysregulation involving type-2 inflammation, altered immune cell balance, and autoantibody formation.
Fernando Carnavali, MD, medical director of the Center for Post-Covid Care at Mount Sinai, believes early intervention could prove crucial.
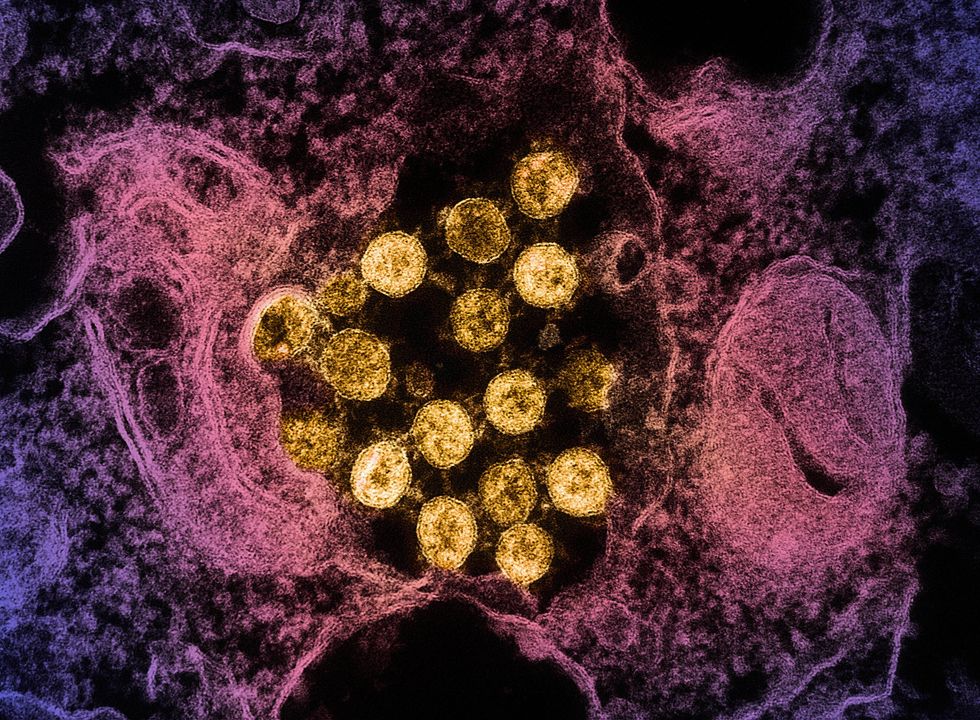
Immune system dysfunction and mast cell activation syndrome may be primary mechanisms driving allergic responses
|GETTY
"Early screening for new or worsening allergies could capture and potentially modify the course of atopic conditions," he said, adding that researchers must determine whether antihistamines or mast cell stabilisers during acute infection might prevent permanent allergic changes.
He called for prospective studies tracking patients from the moment of infection, with particular focus on those with family histories of allergies or atopy.
Al-Aly urged medical education programmes to incorporate knowledge about long Covid's diverse manifestations, including allergies and mast cell activation syndrome.
Our Standards: The GB News Editorial Charter